About Surgical Sterilization
I am forty-two years old. I haven't been able to use hormonal birth control for years because it triggers migraines. I tried the IUD, but my body wouldn't adapt to it and I had to have it removed. My remaining contraception options were barrier methods (i.e. diaphragm, cervical cap, or condoms) or surgical sterilization.
Surgical sterilization for females is known as tubal ligation. Most commonly, the patient is put under general anesthesia. Two incisions are made, through which the surgeon will access each of the fallopian tubes. The tubes will be cut and sealed, either by burning or by using clips. Another method is to access the tubes through the vagina and cervix, and insert implants that will cause scar tissue to develop around them and block the tubes. The patient is considered sterile after her next menstrual period.
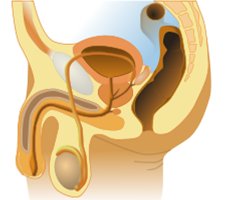
For males, the process is called vasectomy. Under local anesthesia, two small incisions will be made in the scrotum and the surgeon pulls out a loop of vas deferens. Each tube will be cut and sealed with an electrical instrument, or alternatively a small section will be removed and the cut ends tied shut. The process takes about an hour, and the patient can go home right away. He is considered sterile after two successive negative sperm counts, about a month apart. This generally takes 20-25 ejaculations to clear his system of all active sperm.
With either form of surgical sterilization, the goal is to put up a roadblock that keeps sperm and egg from reaching one another. Though it is possible to attempt reversal, in the case of regrets, it is likely to be unsuccessful. Getting surgically sterilized should be considered permanent.
As with all surgeries there are risks of complications, but the risks are higher for female sterilization. The fallopian tubes are deeper inside the body, which makes the surgery more invasive. Both methods have the risk of failure (0.3% for males and 0.5% for females), where the cut ends of the tubes find each other and heal. Either failure could result in an unplanned pregnancy, but if it is a failure in the female's body, then there is an increased chance that the pregnancy will be ectopic - a situation that is life threatening for the pregnant woman. There is a very low chance that this would happen, but it should be part of the consideration when a couple is considering surgical sterilization.
Surgical sterilization for females is known as tubal ligation. Most commonly, the patient is put under general anesthesia. Two incisions are made, through which the surgeon will access each of the fallopian tubes. The tubes will be cut and sealed, either by burning or by using clips. Another method is to access the tubes through the vagina and cervix, and insert implants that will cause scar tissue to develop around them and block the tubes. The patient is considered sterile after her next menstrual period.
For males, the process is called vasectomy. Under local anesthesia, two small incisions will be made in the scrotum and the surgeon pulls out a loop of vas deferens. Each tube will be cut and sealed with an electrical instrument, or alternatively a small section will be removed and the cut ends tied shut. The process takes about an hour, and the patient can go home right away. He is considered sterile after two successive negative sperm counts, about a month apart. This generally takes 20-25 ejaculations to clear his system of all active sperm.
With either form of surgical sterilization, the goal is to put up a roadblock that keeps sperm and egg from reaching one another. Though it is possible to attempt reversal, in the case of regrets, it is likely to be unsuccessful. Getting surgically sterilized should be considered permanent.
As with all surgeries there are risks of complications, but the risks are higher for female sterilization. The fallopian tubes are deeper inside the body, which makes the surgery more invasive. Both methods have the risk of failure (0.3% for males and 0.5% for females), where the cut ends of the tubes find each other and heal. Either failure could result in an unplanned pregnancy, but if it is a failure in the female's body, then there is an increased chance that the pregnancy will be ectopic - a situation that is life threatening for the pregnant woman. There is a very low chance that this would happen, but it should be part of the consideration when a couple is considering surgical sterilization.



To be honest, and this is a bit of a touchy comment to make since it's such a personal article you've written, but - this article scares me quite a bit. Every couple is, of course, different, and you have to do what you believe is right for you. But the idea that surgical sterilization, which to me seems like such an extreme and irreversible path, is the best form of birth control for an unmarried youngish couple, seems a little, well, drastic. What if, God forbid, you were to separate and end up with other people, or just change in the course of your lives? What if you decide later than you would want biological children? I also feel like, at least in the course of the article, you jumped pretty quickly to surgical sterilization as the only acceptable choice of birth control. I realize there may be good reasons for forgoing other methods, but it just seems so extreme a thing to do just to avoid condoms. I guess I don't get what's so bad about condoms, but that's just me. Not trying to judge, but it seems a bit intense.
I am 42, past the age of safe child-bearing and my boyfriend is 52.
I understand your concern, but we are not young and neither of us wants children. Also, pregnancy would not be safe for me for medical reasons. What I didn't go over in the article is how do you know that you don't want children at all? We have been considering our options for several years and are happy that this decision is right for us - it will not be the right decision for everyone.
interesting and informative, I look forward to your future posts in this series